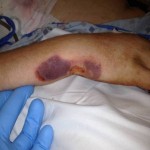
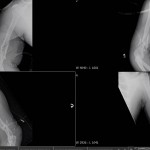
On the day of the injury, the trauma surgical team immediately initiated advanced trauma life support stabilization protocols for trauma resuscitation. They achieved intravenous access and initiated shock treatment. A warmed operating room had been prepared and blood products were ordered for planned rapid infusion. The team placed a chest tube and confirmed the diagnosis of a simple pneumothorax from a penetrating gunshot wound. They performed a brief neurovascular exam of both hands, which suggested Smith suffered no major arterial disruption and all major nerve distributions were sensate. While prepping Smith in the operating theater, the team performed rapid sequence intubation for anesthetic care. The general surgeons performed an exploratory laparotomy while the orthopaedic surgeons performed irrigation and debridement of both upper extremity injuries and multiple soft tissue wounds, and applied negative pressure wound dressing. The surgeons took care to ensure that any penetration to the elbow joint was ruled out via saline arthrogram and direct inspection.
On the second day, the orthopaedic surgeons repeated irrigation and debridement of Smith’s wounds.
Within 72 hours of his injuries, Smith was stabilized and aeromedically evacuated from the theater with both of his arms splinted. He had been extubated and was able to follow commands and demonstrated use of both hands.
He arrived at a hospital outside the combat zone and was recovering well from his chest and abdominal wounds. Surgeons continued repeat irrigation and debridement of his open wounds. Five days after he was injured, Smith arrived at a stateside tertiary care military hospital and received repeated irrigation and debridement of his wounds.
At this point, what plan would you recommend for definitive care of Smith’s injuries? What concerns would you have for the positioning and approach? Would you fix both sides at once?